Common symptoms
- Headache: The most common symptom, it’s caused by an increased pressure in the brain
- Hemiparesis
- Nausea
- Seizure
- Progressive memory
- Personality deficit
- Vomiting
The kind of symptoms produced depends highly on the location of the tumour.
Diagnosis
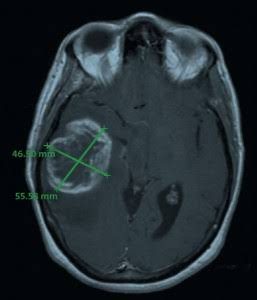
Sophisticated imaging techniques can very accurately pinpoint the location of brain tumors. Diagnostic tools include computed tomography (CT or CAT scan) and magnetic resonance imaging (MRI).
Surgery
The first treatment step is surgery to remove as much tumour as possible. Surgery is almost always followed by radiation. As glioblastoma wildly invade and infiltrate normal surrounding brain tissue it is impossible to completely excise the tumour. The primary objective of surgery is to remove as much of the tumor as possible without injuring the surrounding normal brain tissue needed for normal neurological function (such as motor skills, the ability to speak and walk, etc.). However, GBMs are surrounded by a zone of migrating, infiltrating tumor cells that invade surrounding tissues, making it impossible to ever remove the tumor entirely. Surgery, provides the ability to reduce the amount of solid tumor tissue within the brain, remove those cells in the center of the tumor that may be resistant to radiation and/or chemotherapy and reduce intracranial pressure. Surgery, by providing a debulking of the tumor, carries the ability to prolong the lives of some patients and to improve the quality of remaining life.
Radiotheraphy
After surgery, when the wound is healed, radiation therapy can begin. The goal of radiation therapy is to selectively kill the remaining tumor cells that have infiltrated the surrounding normal brain tissue. In standard external beam radiation therapy, multiple sessions of standard-dose “fractions” of radiation are delivered to the tumor site as well as a margin in order to treat the zone of infiltrating tumor cells.
Chemotheraphy
Patients undergoing chemotherapy are administered special drugs designed to kill tumor cells. Chemotherapy with the drug Temozolomide is the current standard of treatment for GBM. The drug is generally administered every day during radiation therapy and then for six to 12 cycles after radiation. Each cycle lasts for 28 days, with Temozolomide given the first five days of each cycle, followed by 23 days of rest. While the aim of chemotherapy is long-term tumor control, it does so in only about 20 percent of patients. The decision to prescribe other forms of chemotherapy for tumor recurrence is based on a patient’s overall health, type of tumor and extent of the cancer. Before considering chemotherapy, patients should discuss it with their oncologists and/or neuro-oncologists.
Because surgery, radiation and chemotherapy are unlikely to result in a prolonged remission of GBM tumors, researchers are always investigating the use of innovative new treatments when the first line therapy has failed. These new treatments are done in clinical trials. A number of these treatments are available on an investigational basis at centers specializing in brain-tumor therapies. These include gene therapy, highly focused radiation therapy, immunotherapy and chemotherapies utilized in conjunction with vaccines.
For brain tumour patients, a prognosis depends on several factors, which can include age and other health issues, the size of the tumour, its molecular profile, the type of tumour, how much can be removed and its response to treatments such as chemotherapy and radiation therapy.
For adults with glioblastoma, treated with temozolomide chemotherapy and radiation therapy at the same time, median survival is about 14.6 months and two-year survival accounts for 30% of patients. However, a 2009 study reported that almost 10% of patients with glioblastoma may live five years or longer.