Location
Although meningiomas are referred to as brain tumors, they do not grow from brain tissue. They arise from the meninges, which are three thin layers of tissue covering the brain and spinal cord. These tumors are most often found near the top and the outer curve of the brain. Tumors may also form at the base of the skull.
Different Location in The brain are
- Convexity (surface of the brain) (19%)
- Falx and Parasagital (25%)
- Sphenoid ridge (17%)
- Suprasellar (9%)
- Olfactory groove (8%)
- Posterior fossa (8%)
- Middle fossa (4%)
- Tentorial and Peri-torcular (4%)
- Intraventricular (1%)
- Intraorbital (1%)
Convexity meningiomas
These grow on the surface of the brain, often toward the front. They may not produce symptoms until they reach a large size. Symptoms of a convexity meningioma are seizures, focal neurological deficits such as monoparesis, hemiparesis, or headaches.
Falx and Parasagittal meningiomas
The falx is a groove that runs between the two sides of the brain i.e. cerebral hemisphere, and contains a large blood vessel (sagittal sinus). Parasagittal tumors lie near or close to the falx. Because of the danger of puncturing the blood vessels, removing a tumor in the falx or parasagittal region can be difficult. Large parasagittal meningiomas may result in bilateral leg weakness.
Olfactory groove meningiomas
Olfactory groove meningiomas grow along the nerves that run between the brain and the nose. These nerves allow you to smell, and so often tumors growing here cause loss of smell. If they grow large enough, olfactory groove meningiomas can also compress the nerves to the eyes, causing visual symptoms. Similarly, meningiomas growing on the optic nerve can cause visual problems, including loss of patches within your field of vision, or even blindness. They can grow to a large size prior to being diagnosed due to changes in the sense of smell and mental status changes being difficult to recognize.
Sphenoid meningiomas and Middle fossa meningiomas
These meningiomas lie behind the eyes. These tumors can cause visual problems, loss of sensation in the face, or facial numbness. Tumors in this location can sometimes involve the blood sources of the brain (e.g. cavernous sinus, or carotid arteries), making them difficult or impossible to remove completely.
Suprasellar meningiomas
Suprasellar meningiomas grows in central part of brain above the sella which contains pituitary gland. They compress and displaces optic nerve and causes visual loss. They can also grow and invade important arteries supplying blood flow to the brain such as Internal carotid artery and its branches namely Middle cerebral artery and Anterior cerebral artery making their total resection difficult and some times impossible.
Posterior fossa meningiomas
Posterior fossa tumors lie on the underside of the brain. These tumors can compress the cranial nerves causing facial symptoms or loss of hearing. Petroclival tumors can compress the trigeminal nerve, resulting in sharp pain in the face (trigeminal neuralgia) or spasms of the facial muscles.
Tentorial Meningiomas and Peritorcular Meningiomas
These arises in posterior part of brain can cause headaches, or other signs cerebellar compression such as difficulty walking.
Intraventricular meningiomas
Intraventricular meningiomas are associated with the connected chambers of fluid that circulate throughout the central nervous system. They can block the flow of this fluid causing pressure to build up, which can produce headaches and dizziness.
Intraorbital meningiomas
Intraorbital meningiomas grow around the eye sockets of the skull and can cause pressure in the eyes to build up, resulting in a bulging appearance. They can also cause an increasing loss of vision.
Spinal meningiomas
Spinal meningiomas account for less than 10 percent of meningiomas. They tend to occur in women (with a female/ male ratio of 5 to 1), usually between the ages of 40 and 70. They are intradural (within or enclosed within the dura mater), extramedullary (outside medulla or spinal cord) tumors occurring predominantly in the thoracic spine. They can cause back pain, or pain in the limbs from compression of the nerves where they run into the spinal cord.
Histological Classification of meningiomas are based upon the WHO classification system.
- Benign (Grade I) – (90%) – meningothelial, fibrous, transitional, psammomatous, angioblastic
- Atypical (Grade II) – (7%) – chordoid, clear cell, atypical (includes brain invasion)
- Anaplastic/malignant (Grade III) – (2%) – papillary, rhabdoid, anaplastic (most aggressive)
Incidence
Meningiomas account for about 36.1% of all primary brain tumors, which are tumors that form in the brain or its coverings. They are most likely to be found in adults older than 60; the incidence appears to increase with age. Rarely are meningiomas found in children. They occur about twice as often in women as in men.
Cause
Researchers are studying meningiomas carefully to find out what causes them. Between 40% and 80% of meningiomas contain an abnormal chromosome 22. The cause of this abnormality is not known.
Meningioma Symptoms
Meningiomas usually grow slowly, and may reach a large size before interfering with the normal functions of the brain. The resulting symptoms depend on the location of the tumor within the brain. The most common symptoms are,
- Headaches
- Seizures
- Blurred vision
- Personality changes
- Weakness in arms or legs
- Numbness
- Speech problems
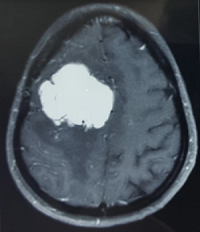
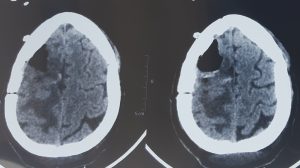
Diagnosis of Meningiomas
Meningiomas are rarely diagnosed before they begin to cause symptoms. Meningiomas are visualized readily with contrast CT, MRI with gadolinium.
Treatment
Surgery and radiation are the most common forms of treatment for meningioma.
Surgery
Surgery is the primary treatment for meningiomas, although some tumors may not be removed this way. For tumors in favourable locations, up to 85% of meningiomas are curable with surgery. Location, the amount of the tumor left after surgery, and the skill of the neurosurgeon are the important elements in predicting a successful result.
Extent of removal
The major clinical factor in recurrence is the extent of resection/ removal. How completely the surgeon is able to remove the tumor is highly impacted by the location of the tumor, whether it is adjacent or attached to anything else, and the age of the patient. The probability of a tumor recurring or growing after surgery may be estimated by comparing the tumour’s WHO (World Health Organization) grade and by the extent of surgery by the Simpson Criteria.
| Simpson Grade | Completeness of Resection |
| Grade I | complete removal including resection of underlying bone andassociated dura |
| Grade II | complete removal and coagulation of dural attachment |
| Grade III | complete removal without resection of dura or coagulation |
| Grade IV | subtotal resection |
Radiation therphy
Radiation therapy may be used to tumors that cannot be removed with surgery, tumors that are not completely removed in surgery, malignant/anaplastic tumors, or recurrent tumors.
Observation
Careful observation is sometimes the best course of action for patients with meningioma with small incidentally detected tumour on imaging done for other purpose or with old age or if surgery is not possible due to other comorbidities. Scans are performed at regular intervals during this time.
Prognosis
For tumors in favourable locations, up to 85% of meningiomas are curable with surgery. Location, the amount of the tumor left after surgery, and the skill of the neurosurgeon are the important elements in predicting a successful result.